Diabetic retinopathy (DR) is a leading cause of preventable blindness among adults.1
In 2020, it was estimated that more than 103 million adults worldwide had DR.2 It can develop in anyone who has type 1 or type 2 diabetes, and is caused by damage to the blood vessels of the light-sensitive tissue at the back of the eye.3 Risk increases the longer a person has diabetes. More than half of people who have diabetes will develop DR.4
This progressive disease can lead to irreversible vision loss. One of the most troubling aspects of DR is that people often have no symptoms early on. Unfortunately, a lack of symptoms doesn’t indicate a lack of damage. It’s often not until the later stages of the disease that vision loss becomes apparent. Early diagnosis can help slow the progression and preserve sight. That’s why it’s critical for those who have diabetes to get regular eye exams — even if their vision seems fine.
“It’s important to stress how silent it can be,” said Dr. Grayson Armstrong, an ophthalmologist at Massachusetts Eye and Ear in Boston. “Patients can be asymptomatic for years and have developed worsening symptoms by the time you see them.“
Common DR symptoms include5:
- Floating spots or streaks
- Blurred vision
- Fluctuating vision
- Dark or empty areas of vision
- Vision loss
The importance of eye exams
The American Diabetes Association recommends that adults with type 2 diabetes have eye exams when they’re diagnosed.6 Those who have type 1 diabetes should have eye exams within five years of their diagnosis.7 Following their initial exams, all patients with diabetes should have annual eye exams.8 The problem is only about half of these patients receive recommended annual eye exams.9 The remainder are at high risk for sight-threatening DR, yet many lack knowledge about the disease and the importance of preventive eye care.10 In the absence of symptoms, they may not perceive a need to be screened. Of course, these patients should be screened, even if they don’t have noticeable vision problems.
Other factors for skipping eye exams include insurance status, childcare responsibilities, financial and logistical challenges, lack of time off work and a reluctance to hear more “bad news” about their health. Fear of dilated eye exams is also often a deterrent.
“When DR is caught early, it’s incredibly treatable with new forms of medication to halt progression or reverse the stages of retinopathy, thus preserving patient’s vision.” said Dr. Blake Cooper, a retina specialist at Retina Associates in Kansas City, MO. “It’s important for them to be screened, so they can be identified and referred appropriately.”
Ophthalmologist shortage
Compounding these barriers is a shortage of ophthalmologists. Elderly, high-risk populations who need eye care are increasing while trained physicians who can care for them are dwindling.11 In 2016, the U.S. Health Resources and Services Administration estimated there will be a demand for approximately 22,000 ophthalmic surgeons by 2025.12
It also estimated the number of available ophthalmologists would fall short of that demand by more than 6,000 doctors. Rural areas, in particular, are experiencing less availability.
Now is the ideal time for a new approach; one that helps ensure patients with diabetes get timely access to the care they need.
Closing the DR care gap
Those at the highest risk for vision loss are the same people who could preserve their sight with timely intervention. A novel approach to closing this gap starts with primary care. Adults with diabetes typically see their PCPs more often than their specialists. If PCPs perform retinal screenings during routine exams, they can ease the care gap by detecting and diagnosing DR early. Early intervention is key to preventing vision loss. Performing vision screenings in a primary care setting can overcome many barriers that interfere with prompt treatment.
“It’s not hard for primary care physicians to understand their [diabetic] patients will develop retinopathy and need to be screened,” said Dr. Blake Cooper. “Now, they have a tool that can do that for them.” Until recently, PCP DR screening may not have been a viable option. Technology advancements, federal regulatory approval and reimbursement policies have not only made it possible, but also easy and costeffective. Today, PCPs can perform DR screenings in their offices during routine patient exams quickly — and without dilation.
Handheld fundus cameras with AI enable widespread access
Handheld fundus cameras take photos of the retina and use artificial intelligence (AI) to evaluate the extent of damage to blood vessels, which is the cause of sightthreatening DR. Automated point-of-care DR screening has high diagnostic accuracy, sensitivity, and specificity and often surpasses human readings. The cameras are portable, can be taken anywhere, and dilation isn’t needed. This groundbreaking technology offers significant advantages over traditional screening techniques because it’s noninvasive, extremely accurate and requires significantly less training than the direct ophthalmoscope.
“Showing someone a picture of their eye is very tangible,” Armstrong said. “Patients might take more onus to control their disease, be more motivated to intervene, and be more compliant with the treatments, medications and follow-up.”
PCPs and other healthcare professionals, including physician assistants, nurse practitioners, nurses and medical assistants, can perform the screening in minutes in any room. Patients get results while on-site and can drive themselves home immediately afterward. When the technology detects DR, PCPs can refer patients to eye care specialists for follow-up. DR screening is slowly coming into the primary care setting, given FDA approved technologies for automated AI-based DR detection and favorable reimbursement policies. Because DR is often an untapped revenue stream, many PCP clinics find that this, alone, enables them to quickly recoup and even surpass any initial investment. In addition, DR screening is considered a public health priority and has been incorporated into quality measures, such as the Meritbased Incentive Payment System.13 It might not be long before wellness exams and other routine PCP visits include DR screenings for patients with diabetes. The technology could help transform eye care, especially for those who might otherwise go undiagnosed.
Real-time DR screening reimbursement
- CPT 92229 provides reimbursement for real-time DR screening in patients with diabetes using AI. It covers unilateral or bilateral imaging at the point of care.14
Optomed Aurora AEYE
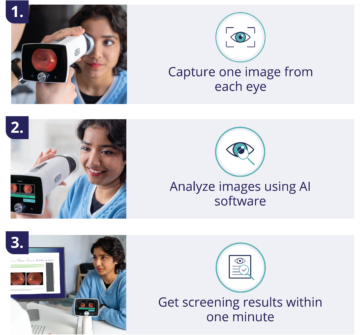
Optomed, a Finnish medical technology company, develops solutions to prevent avoidable blindness and is a leading provider of handheld fundus cameras. The company’s Optomed Aurora AEYE is an FDA-cleared handheld artificial intelligence fundus camera that provides accurate on-the-spot DR detection at the point of care in less than 60 seconds.15 The camera is easy to use and provides excellent clinical results with 92-93% sensitivity, 89%-94% specificity and more than 99% imageability.16 The Optomed Aurora AEYE features autofocus/autoexposure, and no pupil dilation is needed. It detects DR when the AI identifies signs indicating more than mild DR. With training, PCPs and their healthcare professionals can provide vital DR screenings during routine patient exams. To get started, they simply need to purchase Optomed’s handheld fundus camera with integrated AI software and portal. Optomed provides in-person and virtual training. Once a clinic is registered and the team is trained, the clinic can begin imaging patients. The technology is affordable with no startup costs, a low monthly rental fee, and unlimited use.
How AI works
Next-level patient care
AI-based DR imaging helps PCPs and other healthcare professionals close the care gap for vulnerable patients with diabetes while adding a new revenue stream. With regular DR screenings and diabetes management, patients have a much better chance for maintiaing thier vision.
