Benefits of Optomed Aurora IQ in Neurology
A handheld non-mydriatic fundus camera makes ocular fundus examination more accessible in various non-ophthalmology settings. Aurora IQ enables effective and reliable fundus examination and documentation of findings.
High Success Rate
- No need to dilate pupil – saves time and enables monitoring of pupil reactivity
- Photographs can be reliably taken by non-physician staff1
- The success rate of 93% for handheld fundus camera compared to 58% for direct ophthalmoscopy in neurology emergency patients2
- Increased certainty in fundus examination allows for better clinical decisions and patient management3

Patient Friendly
- Handheld operation enables bedside examination of patients unable to sit up
- No need for uncomfortable pupil dilation
- No continuous light to the eye
- No need to re-examine the fundus since the image can be re-analyzed

Documentation
- Fundus image can be saved to electronic medical records
- Allows ophthalmology consulting
- Enables follow-up of treatment progress
- A thorough review of the fundus image on a computer screen
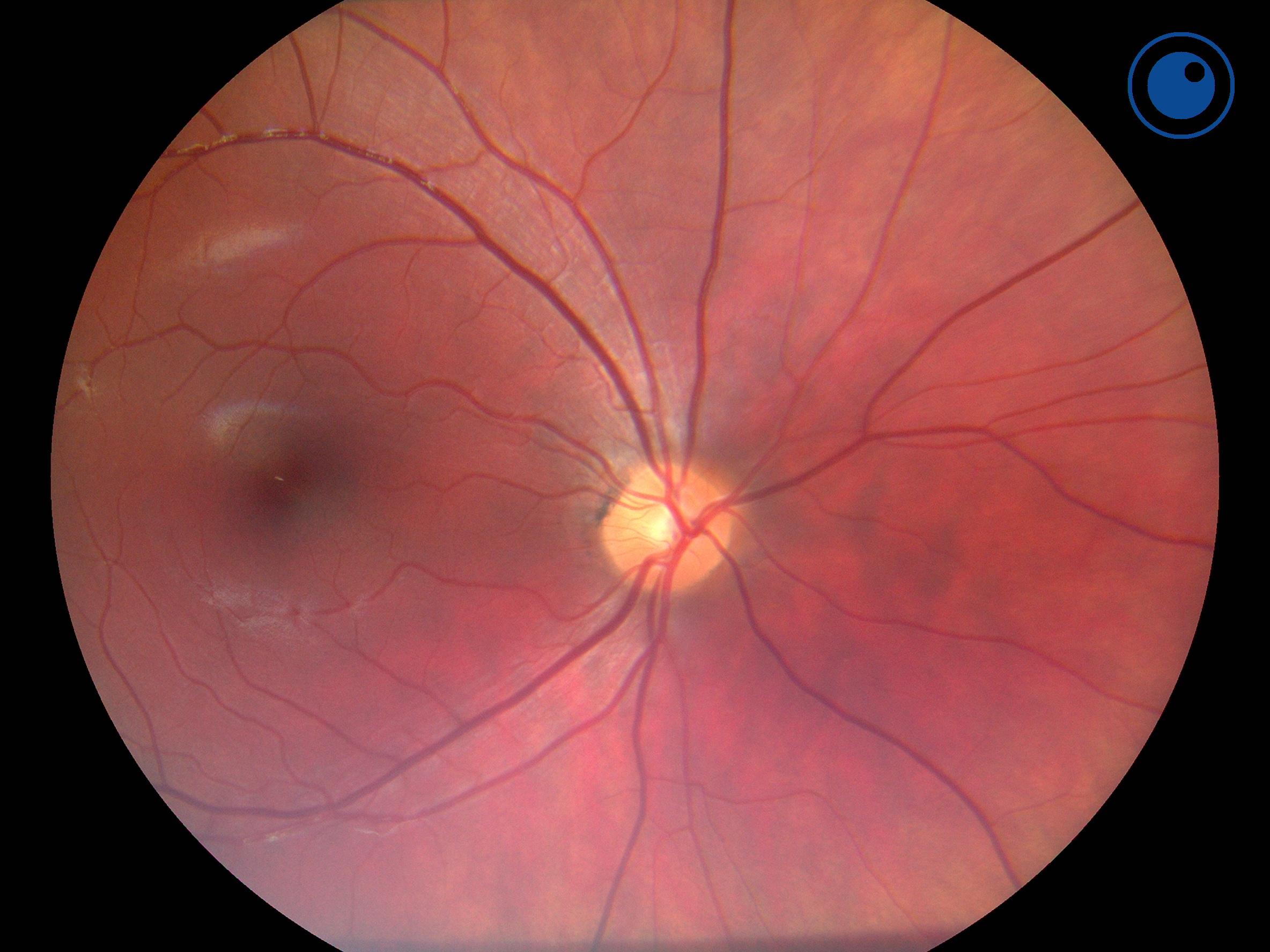
Fundus imaging can be used to diagnose4
- papilledema caused by elevated intracranial pressure
- microvascular changes related to stroke and transient ischemic attack
- hypertensive retinopathy
- optic nerve changes related to ischemic optic neuropathy or optic neuritis
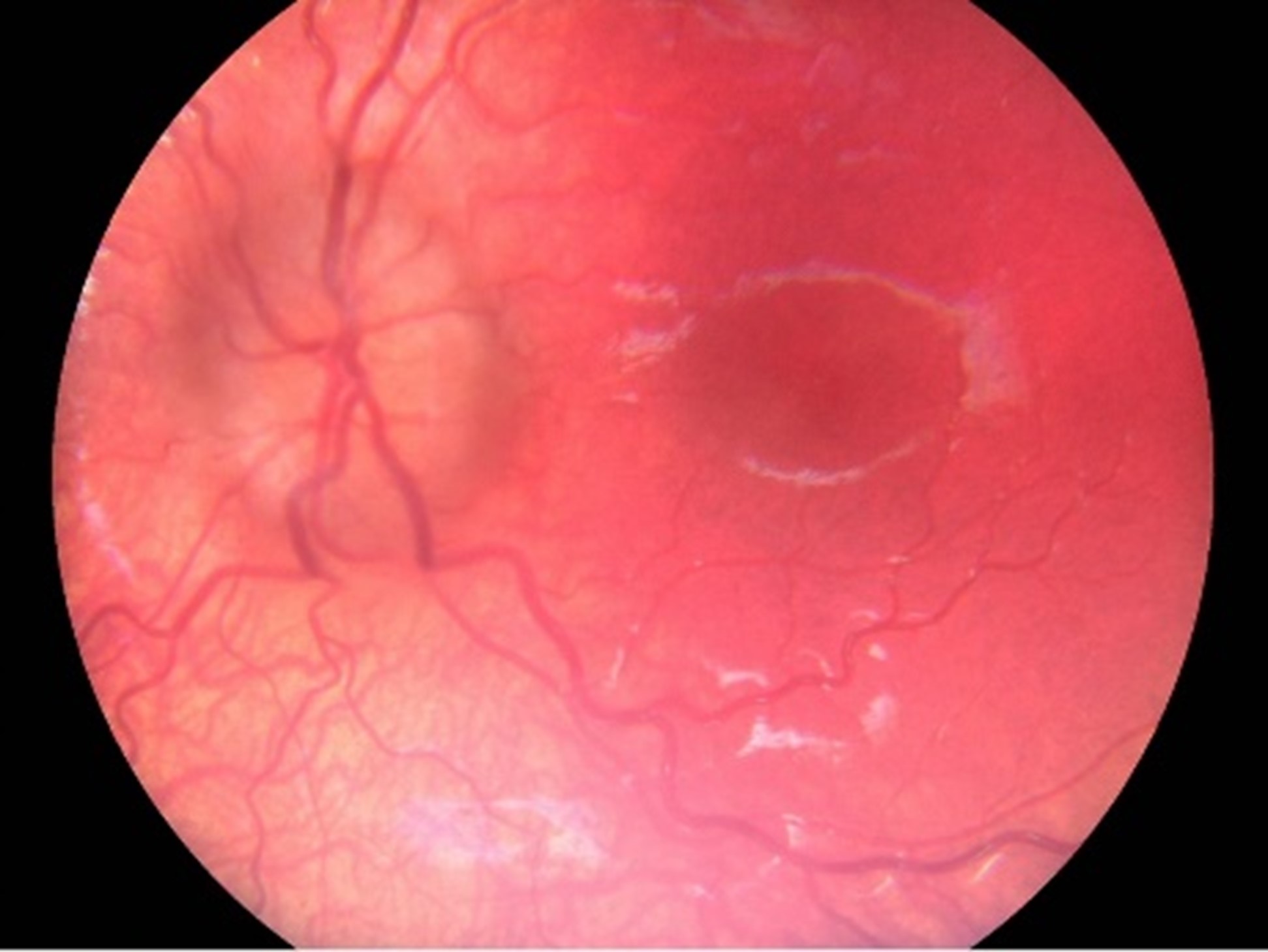
Document anterior segment findings
Aurora IQ brings versatility to the emergency department ophthalmic examinations with both anterior and posterior modules in one device.
Obtain professional ophthalmic quality anterior segment images and save them to electronic medical records. Document ocular emergencies and other anterior segment conditions with high-quality contrast images, with both color and cobalt blue fluorescein modes.

Sources: 1) Pérez MA, Bruce BB, Newman NJ, Biousse V. The use of retinal photography in nonophthalmic settings and its potential for neurology. Neurologist. 2012 Nov;18(6):350-5. 2) Alm M, Hautala N, Bloigu R, Huhtakangas J. Comparison of optic disc evaluation methods in neurology emergency patients. Acta Neurol Scand. 2019 Dec;140(6):449-451. 3) Dunn HP, Browning SD, Thomson D, Yates WB, McCluskey P, Keay L, White AJ, Fraser CL. Impact on patient management of non-mydriatic fundus photography compared to direct ophthalmoscopy in a regional Australian emergency department. Emerg Med Australas. 2021 Aug 27. 4) Mackay DD, Bruce BB. Non-mydriatic fundus photography: a practical review for the neurologist. Pract Neurol. 2016;16(5):343-351.